3 Indicators You Might Need a Heart Valve Replacement
Heart valve problems can develop gradually, making them difficult to detect without medical attention. Understanding the warning signs that might indicate the need for valve replacement can help patients seek timely medical intervention. While not all valve issues require surgery, recognizing these key indicators could potentially be life-saving.
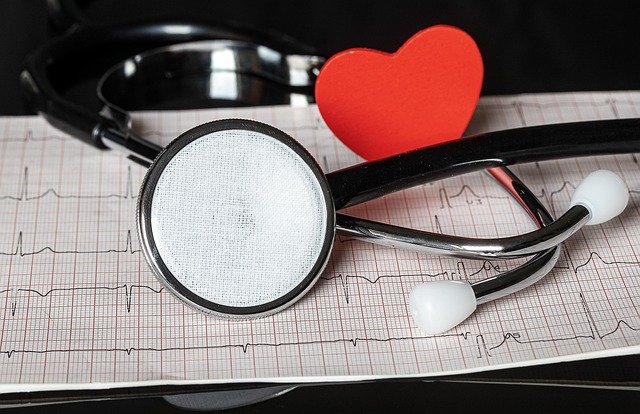
Heart valve disease affects millions of people worldwide and occurs when one or more of your heart’s four valves don’t function properly. These valves ensure blood flows in the correct direction through your heart. When they malfunction, your heart must work harder, potentially leading to serious complications if left untreated. While some valve conditions can be managed with medication and lifestyle changes, others may require surgical intervention, including valve replacement. Recognizing the signs that might indicate the need for such a procedure is crucial for timely medical care.
Shortness of Breath and Decreased Exercise Tolerance
One of the most common signs you might need a heart valve replacement is experiencing shortness of breath, particularly during physical activity or when lying flat. This symptom occurs because a damaged valve can cause blood to back up into your lungs or prevent efficient blood flow through your heart.
Initially, you might notice this breathlessness only during strenuous activities. However, as valve disease progresses, even mild exertion like walking short distances or climbing stairs might leave you winded. Many patients describe needing to sleep with additional pillows (a condition called orthopnea) because lying flat worsens their breathing difficulties.
This decreased exercise tolerance happens because your heart cannot efficiently pump blood when valves aren’t functioning properly. Your body’s tissues and organs don’t receive adequate oxygen, leading to fatigue and breathlessness even with minimal effort. If you notice a significant change in your ability to perform activities you previously handled with ease, this could indicate worsening valve function that might eventually require replacement.
Chest Pain, Palpitations, and Irregular Heartbeat
Heart valve problems often manifest through chest discomfort, palpitations, or irregular heartbeat patterns. These symptoms occur because your heart is working harder to compensate for the malfunctioning valve, potentially causing strain on the heart muscle.
Chest pain related to valve disease might feel like pressure or tightness, particularly during physical activity. Unlike the crushing pain associated with heart attacks, valve-related discomfort often develops gradually and may be accompanied by other symptoms. Some patients describe feeling their heart racing, fluttering, or skipping beats—sensations known as palpitations.
An irregular heartbeat (arrhythmia) can develop as a complication of valve disease. When valves don’t close properly, allowing blood to flow backward (regurgitation), or don’t open fully, restricting blood flow (stenosis), your heart’s electrical system may become disrupted. If you experience persistent or recurrent chest discomfort, palpitations, or notice irregular heart rhythms, these could be signs that your valve condition has progressed to a point where replacement might be necessary.
Swelling, Fatigue, and Signs of Heart Failure
Advanced valve disease can eventually lead to heart failure symptoms, which include fluid retention, extreme fatigue, and decreased kidney function. These symptoms develop when your heart can no longer effectively pump blood throughout your body.
Swelling (edema) typically appears in the ankles, feet, and legs because gravity causes excess fluid to pool in these areas when your heart isn’t pumping efficiently. Some patients also notice abdominal swelling or unexpected weight gain due to fluid retention. This occurs because blood backs up when it can’t flow properly through damaged valves, causing pressure increases in your veins.
Persistent fatigue that isn’t relieved by rest can indicate your heart is struggling to provide adequate blood flow to your body’s tissues. You might feel exhausted even after a full night’s sleep or find yourself needing frequent naps. Some patients describe this fatigue as overwhelming and unlike normal tiredness.
Decreased kidney function may manifest as reduced urination during the day but increased urination at night. Your kidneys may not receive adequate blood flow during the day due to your heart’s compromised pumping ability, but when you lie down at night, fluid redistribution can temporarily improve kidney perfusion.
Diagnostic Process for Heart Valve Problems
If you’re experiencing any of these symptoms, your doctor will likely recommend several diagnostic tests to evaluate your heart valve function. The process typically begins with a thorough physical examination, during which your doctor will listen for heart murmurs—abnormal sounds created by turbulent blood flow through damaged valves.
An echocardiogram is the primary diagnostic tool for valve assessment. This ultrasound examination provides detailed images of your heart’s structure and function, allowing doctors to see how your valves are working. Additional tests might include an electrocardiogram (ECG), chest X-ray, cardiac MRI, or cardiac catheterization, depending on your specific situation.
Your doctor will evaluate the severity of your valve disease, your overall health, and how your symptoms impact your quality of life when determining whether valve replacement is necessary. Not everyone with valve disease requires surgery, but when symptoms significantly affect daily activities or pose risks for complications, replacement may be recommended.
Types of Heart Valve Replacement Procedures
If your doctor determines that valve replacement is necessary, you’ll have options regarding the type of procedure and replacement valve. Understanding these choices can help you participate in treatment decisions.
Surgical valve replacement has been the standard approach for decades and involves open-heart surgery. During this procedure, the surgeon makes an incision in your chest, stops your heart temporarily (using a heart-lung machine to maintain circulation), removes the damaged valve, and replaces it with either a mechanical or biological valve.
Transcatheter valve replacement is a newer, less invasive option that may be suitable for some patients, particularly those at high risk for complications from open surgery. This approach involves threading a replacement valve to your heart through a catheter, typically inserted through a blood vessel in your leg.
Replacement valves come in two main types:
| Valve Type | Durability | Anticoagulation Needs | Best For |
|---|---|---|---|
| Mechanical | 20+ years | Lifelong blood thinners required | Younger patients who can take anticoagulants |
| Biological (tissue) | 10-15 years | Short-term or no blood thinners | Older patients or those who cannot take anticoagulants |
Prices, rates, or cost estimates mentioned in this article are based on the latest available information but may change over time. Independent research is advised before making financial decisions.
Recovery and Long-term Outlook
Recovery following valve replacement varies depending on the surgical approach and your overall health. Traditional open-heart procedures typically require a hospital stay of 4-7 days and a recovery period of 6-8 weeks before returning to normal activities. Minimally invasive procedures often allow for faster recovery, with some patients returning home within a few days.
Long-term outcomes for valve replacement are generally excellent, with most patients experiencing significant symptom improvement and enhanced quality of life. However, regular follow-up appointments are essential to monitor valve function and address any complications promptly.
Lifestyle modifications after valve replacement typically include cardiac rehabilitation, a heart-healthy diet, regular exercise as recommended by your doctor, and medication management. Patients with mechanical valves will need lifelong anticoagulation therapy to prevent blood clots from forming on the valve.
Heart valve replacement has evolved significantly over recent decades, with technological advances continually improving outcomes and expanding options for patients. Recognizing the signs that might indicate the need for valve replacement and seeking prompt medical attention when symptoms develop are crucial steps in managing heart valve disease effectively.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.