how to detect EB Disease and explore new approaches emerging in 2025
Epidermolysis Bullosa (EB) presents unique challenges for seniors and their caregivers. This rare genetic disorder causes fragile skin that blisters easily, requiring specialized detection methods and treatment approaches. As medical science advances, new diagnostic techniques and therapeutic options are emerging that offer hope for improved management and quality of life for those affected by this complex condition.

Epidermolysis Bullosa (EB) is a group of rare genetic disorders characterized by extremely fragile skin that blisters and tears from minor friction or trauma. While typically diagnosed in infancy, some milder forms may not be identified until later in life, making awareness particularly important for senior health. Early and accurate detection is crucial for proper management, especially as innovative approaches are being developed for 2025 and beyond. This article explores current diagnostic methods and emerging treatments for EB disease.
Understanding Epidermolysis Bullosa and Its Symptoms
Epidermolysis Bullosa manifests primarily through skin fragility and blister formation. In seniors, symptoms may include recurring blisters on the hands, feet, and pressure points, wounds that heal slowly or with scarring, nail abnormalities, and in some cases, internal blistering affecting the mouth, esophagus, or other mucous membranes. There are four main types of EB: simplex, junctional, dystrophic, and Kindler syndrome, each with varying severity and characteristics. For older adults who develop symptoms later in life or have lived with undiagnosed milder forms, recognizing these patterns can lead to proper medical evaluation and improved quality of life through appropriate interventions.
Current Methods for Diagnosing Epidermolysis Bullosa
Accurate diagnosis of EB requires specialized testing beyond standard dermatological examinations. The gold standard for Diagnosing Epidermolysis Bullosa involves skin biopsies examined under electron microscopy to identify the specific layer of skin where separation occurs. Immunofluorescence mapping helps pinpoint the exact proteins affected by genetic mutations. Genetic testing through blood samples can identify the specific gene mutations responsible for the condition, which is crucial for determining the type and subtype of EB. For seniors who may have lived with undiagnosed EB, comprehensive testing is essential as it informs treatment approaches and helps predict potential complications that may become more pronounced with age.
Finding the Right Doctor to Treat EB
Managing EB requires a multidisciplinary approach, particularly for seniors who may have concurrent health conditions. Specialists who commonly treat EB include dermatologists with expertise in genetic skin disorders, wound care specialists, gastroenterologists for internal complications, pain management specialists, and genetic counselors. When seeking a Doctor to treat EB, seniors should look for medical professionals affiliated with specialized EB centers or university hospitals with experience in rare genetic disorders. The EB Clinical Research Consortium and patient advocacy organizations like DEBRA (Dystrophic Epidermolysis Bullosa Research Association) can provide referrals to knowledgeable healthcare providers. Establishing care with a coordinated team is essential for comprehensive management of this complex condition.
Traditional Epidermolysis Bullosa Treatments
Current Epidermolysis Bullosa treatments focus primarily on wound care, pain management, and preventing complications. Standard approaches include gentle wound cleaning and specialized non-adhesive dressings to protect fragile skin and promote healing. Pain management protocols often combine topical and systemic medications tailored to individual needs. Nutritional support is crucial, especially for seniors with oral or esophageal involvement that affects eating. Physical and occupational therapy help maintain mobility and function, particularly important for maintaining independence in older adults. While these treatments don’t cure EB, they significantly improve quality of life by reducing complications and addressing symptoms.
Innovative Approaches to EB Management for 2025
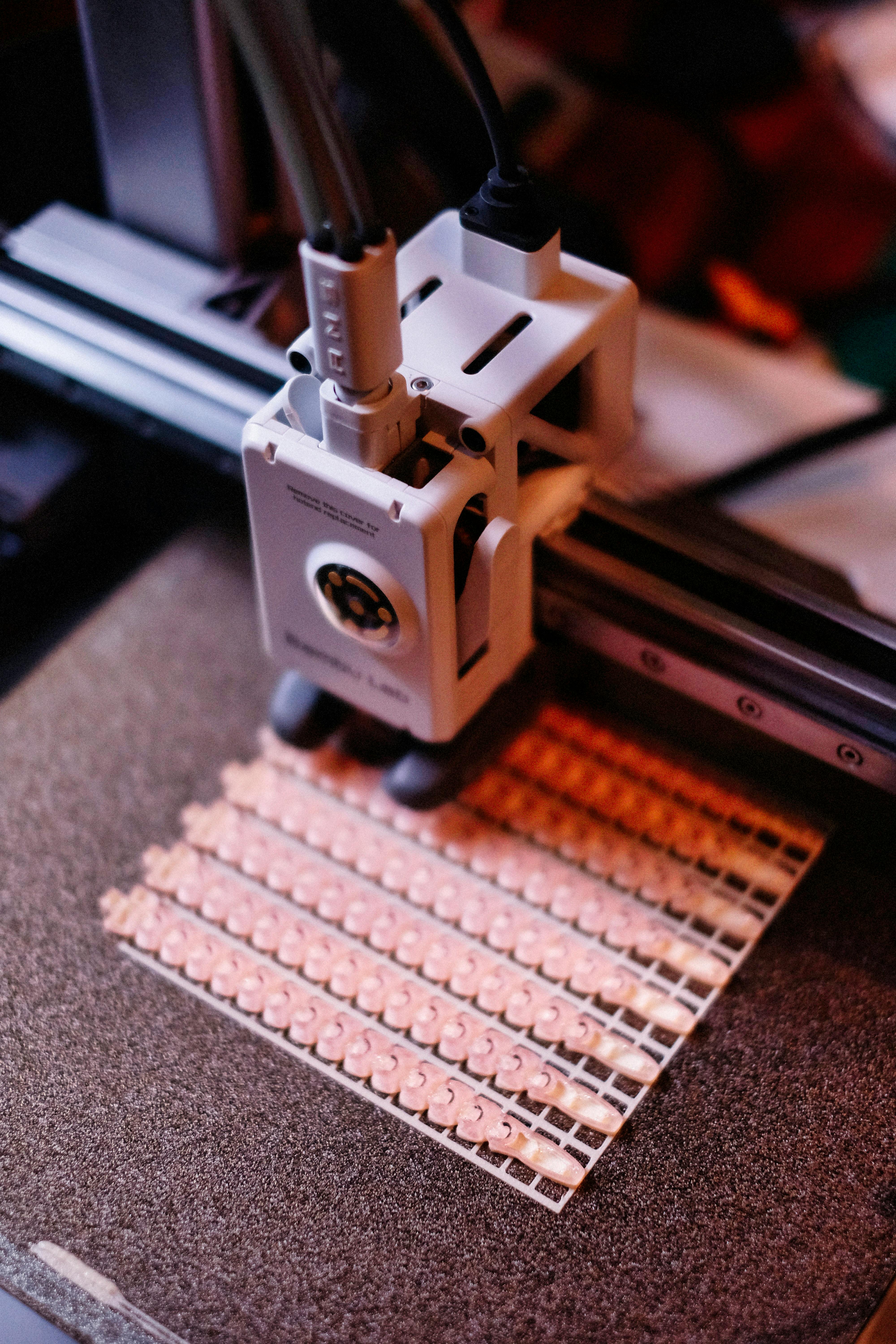
The landscape of EB treatment is evolving rapidly, with several promising approaches expected to advance in 2025. Gene therapy trials are showing potential for correcting the genetic mutations responsible for EB, with techniques like CRISPR-Cas9 gene editing being refined for greater safety and efficacy. Cell-based therapies using modified stem cells to produce functioning proteins are progressing through clinical trials. Protein replacement therapies aim to deliver functioning versions of the defective proteins directly to the skin. Advanced wound care technologies, including specialized bioengineered dressings and skin substitutes, are being developed specifically for EB patients. For seniors with EB, these innovations may offer better symptom management and improved quality of life, even for those with long-standing disease.
Emerging Clinical Trials and Research Initiatives
Research into EB treatments is accelerating, with numerous clinical trials scheduled for 2025. Gene therapy approaches using viral vectors to deliver corrected genes are advancing to later-stage trials. Topical gene therapies that can be applied directly to wounds show promise for localized treatment. Small molecule drug trials are investigating compounds that can modify how cells process defective proteins or enhance the function of compensatory proteins. Several pharmaceutical companies and research institutions have dedicated EB research programs with treatments in various stages of development. Seniors interested in participating in clinical trials should discuss options with their healthcare providers and connect with organizations like the EB Research Partnership or ClinicalTrials.gov to identify suitable studies.
Managing EB in Senior Populations: Special Considerations
Seniors with EB face unique challenges that require specialized approaches. Age-related skin changes, including decreased elasticity and slower healing, can exacerbate EB symptoms. Comorbid conditions common in older adults, such as diabetes or vascular disease, may complicate wound healing. Medication interactions between EB treatments and drugs for other conditions require careful management. Mobility limitations may increase the risk of pressure-related blisters. Healthcare providers should develop comprehensive care plans that address these age-specific factors while considering quality of life and independence. Support services, including home health care and adaptive equipment, can help seniors with EB maintain autonomy while managing their condition effectively.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.